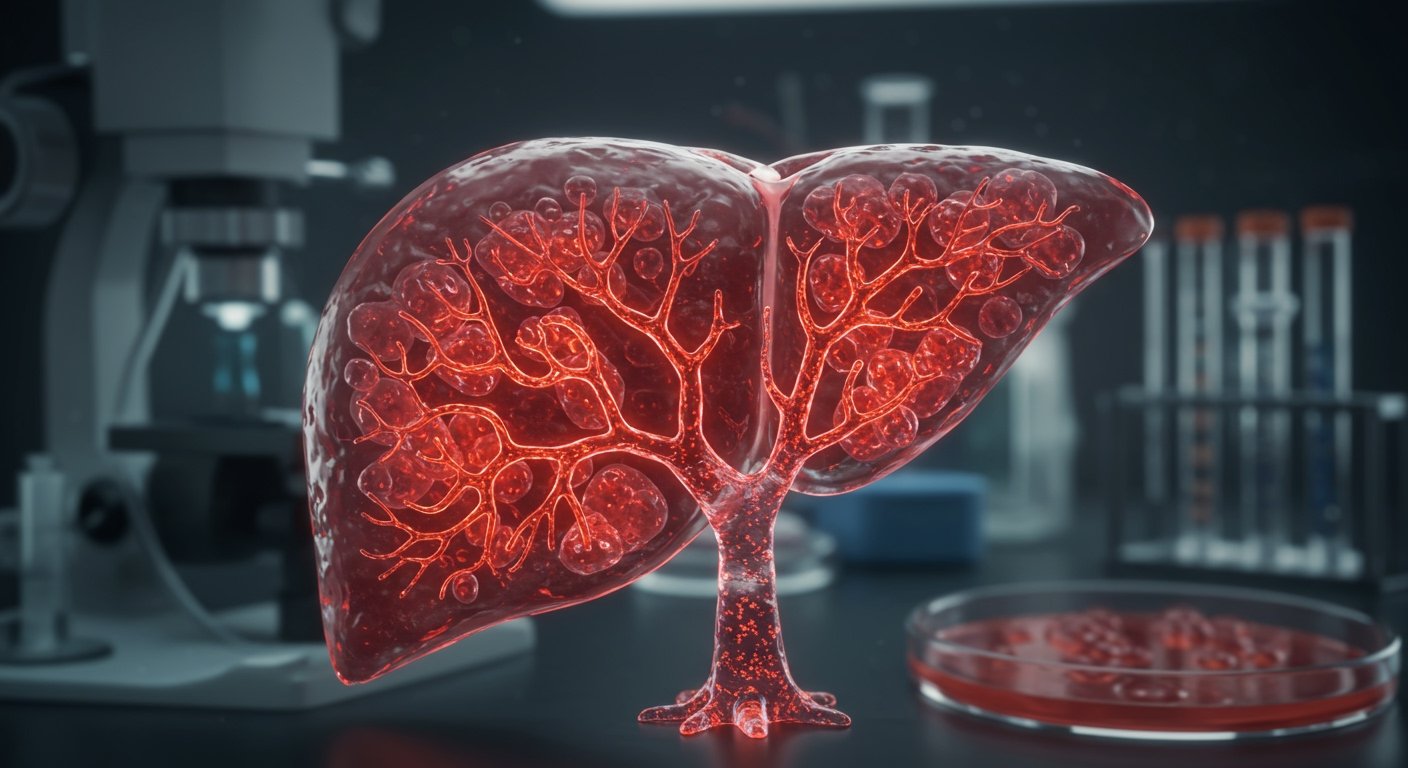
Scientists have achieved a significant breakthrough in regenerative medicine, successfully growing liver organoids – miniature, lab-grown organs – that contain fully functional blood vessels. This development, detailed in the journal Nature Biomedical Engineering, represents a major step towards creating transplantable liver tissues and offers potential new avenues for treating blood-clotting disorders like haemophilia.
Led by Dr. Takanori Takebe, MD, the director for commercial innovation at the Cincinnati Children’s Center for Stem Cell and Organoid Research and Medicine (CuSTOM), the research involved a collaborative effort across multiple institutions. Experts from Cincinnati Children’s Hospital partnered with researchers from the Institute of Science Tokyo, the Icahn School of Medicine at Mount Sinai, and Takeda Pharmaceutical Co. The ability to integrate functional blood vessels into lab-grown tissues has long been a major hurdle in the field, as blood supply is critical for tissue survival and function.
The Challenge of Vascular Integration
Creating organoids that accurately mimic the structure and function of real organs requires overcoming several complex biological challenges. One of the most critical is the development of a vascular network – the system of blood vessels that delivers nutrients and oxygen and removes waste. Without this network, lab-grown tissues are typically limited in size and cannot survive or function effectively for extended periods or when introduced into a living organism.
The team’s success lies in their ability to coax different cell types within the liver organoid to self-organize and form a viable, internal blood vessel system. This intricate integration allows the organoids to mature and perform more complex functions closer to those of a native liver tissue. The findings, published in the prestigious journal Nature Biomedical Engineering, highlight the innovative techniques employed to achieve this level of biological complexity in vitro.
Key Functional Outcomes and Therapeutic Promise
Beyond merely surviving, the researchers demonstrated that these vascularized liver organoids were functionally active, specifically in tasks related to blood coagulation. A key finding was the successful production of four different blood clotting factors by the organoids. Among these was Factor VIII, a crucial protein that is deficient or defective in individuals with haemophilia A, a severe inherited bleeding disorder.
To evaluate the therapeutic potential, the team tested the organoids in mouse models designed to mimic the condition of haemophilia. Introducing the Factor VIII-producing liver organoids into these models resulted in a remarkable outcome: the severe bleeding characteristic of haemophilia was effectively reversed. This experimental success in a living system provides compelling evidence for the potential of these lab-grown tissues as a future therapeutic approach for haemophilia A.
The ability of these organoids to produce vital clotting factors like Factor VIII suggests they could potentially provide a sustained source of these proteins within a patient, offering a more permanent or longer-lasting treatment alternative compared to current protein replacement therapies.
Broader Implications for Transplantation and Regenerative Medicine
The successful integration of functional blood vessels has profound implications extending beyond haemophilia. A primary goal of liver organoid research is to create tissues suitable for transplantation, potentially offering a solution for patients with severe liver disease who require a transplant but face organ shortages.
The vascularization achieved in this study brings the prospect of generating transplantable liver tissue much closer to reality. For such tissues to survive and integrate within a patient’s body, a pre-existing or rapidly formed vascular network is essential to connect with the host’s circulatory system.
Furthermore, the methodology used in this research, specifically the IMALI culture method, appears to be adaptable. The scientists suggest that this technique could be applied to generate organ-specific vasculature in other types of organoids as well. This capability could potentially revolutionize the broader field of regenerative medicine, enabling the creation of more complex, functional tissues for a wide range of organs, including kidneys, lungs, and intestines.
Collaboration Driving Innovation
The complexity of this research underscores the importance of international and interdisciplinary collaboration. The combined expertise from academic institutions like Cincinnati Children’s Hospital, the Institute of Science Tokyo, and the Icahn School of Medicine at Mount Sinai, alongside the resources and focus of a pharmaceutical company like Takeda Pharmaceutical Co., was instrumental in achieving this breakthrough.
Dr. Takebe and his colleagues’ work represents a significant milestone, moving liver organoid technology closer to clinical application. While further research and development are necessary before this can translate into treatments for patients, the successful creation of vascularized, functional liver organoids capable of reversing bleeding in disease models marks a pivotal moment in the quest to develop lab-grown tissues for therapy and transplantation.
This advancement not only holds direct promise for individuals with haemophilia and liver disease but also paves the way for similar breakthroughs across the entire spectrum of regenerative medicine, potentially leading to transformative treatments for numerous conditions in the future.